|
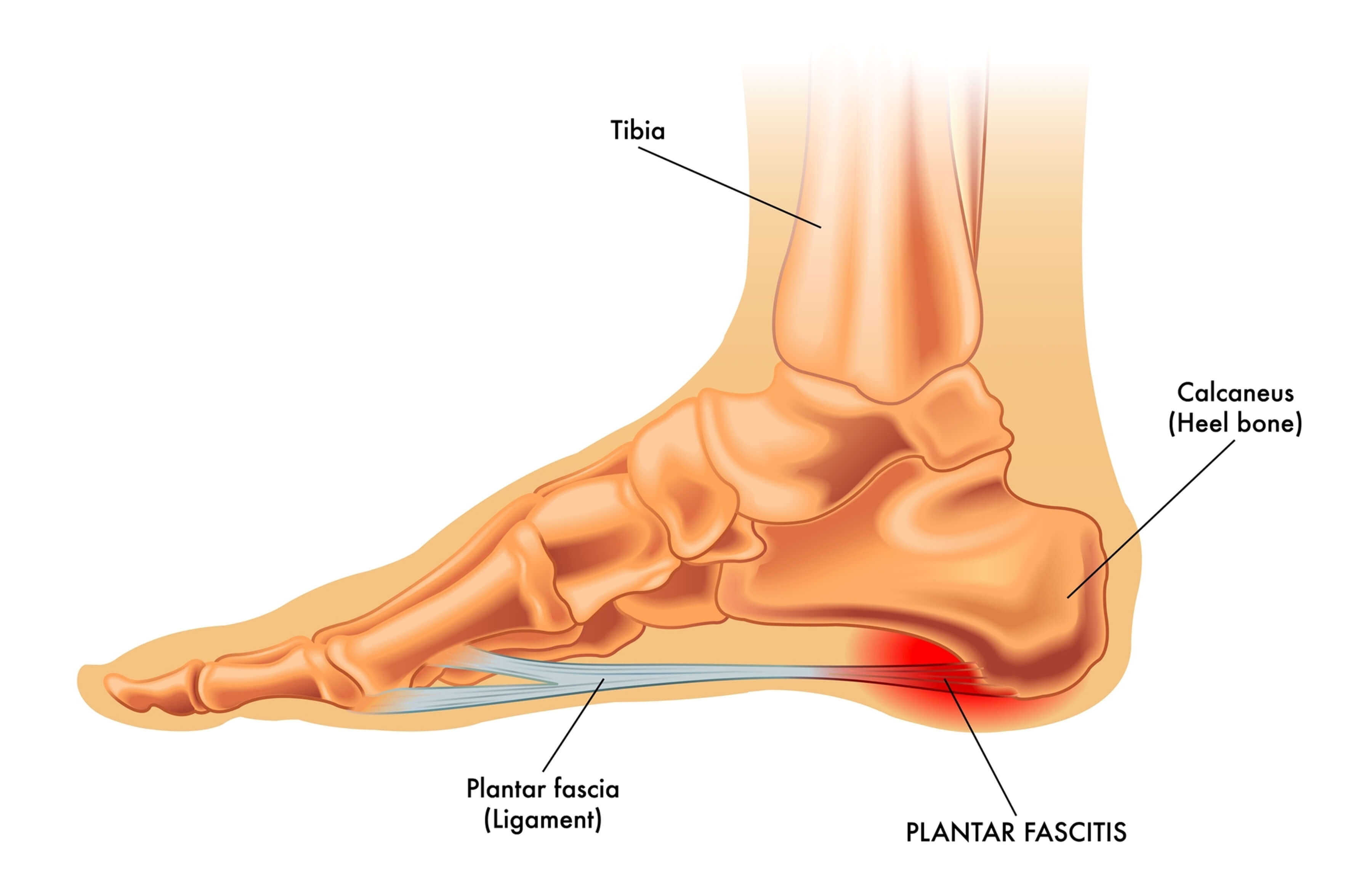
Plantar Fasciitis (or fasciopathy) is a condition of pain and tissue damage at the attachment of the plantar fascia to the underside of the calcaneus (heel bone). |
|
|
|
| ANATOMY | |
|
The plantar fascia is a band of connective tissue that runs along the sole from the heel to the ball of the foot. One of its main roles is to keep the bones and joints in position and enables us to push off from the ground. Bruising or overstretching this ligament can cause inflammation and heel pain. In many cases, plantar fasciitis is associated with a heel spur. Surprisingly, the spur itself does not cause pain, and may often be found in the other foot without symptoms. |
|
| RISK | |
|
|
|
| PREVENTION | |
|
|
| SIGNS & SYMPTOMS | |
|
Pain is usually felt on the underside of the heel, and is often most intense with the first steps of the day or after rest. It is commonly associated with long periods of weight bearing or sudden changes in weight bearing or activity. |
|
|
|
You may experience:
|
| IMMEDIATE MANAGEMENT | |
|
Initial treatment includes gentle stretching of the Achilles tendon and plantar fascia, weight loss, taping, arch support and heel lifts. Difficult cases may be referred for physiotherapy. Physiotherapy includes myofascial release and scar tissue breakdown of the plantar fascia, and supervised stretching. A strengthening program for the calf muscles and small muscles of the foot is important. Be aware that this may increase soreness initially, but persistence should be rewarding. Care should be taken to wear supportive and stable shoes. Patients should avoid open-back shoes, sandals, ‘flip-flops’, and any shoes without raised heels. A podiatrist can assist with plantar fasciitis and other foot and lower limb problems. |
|
| TREATMENT | |
|
For most people, the condition improves spontaneously within a year. Treatments that may help control symptoms include: |
|
|
|
| REHABILITATION AND RETURN TO PLAY | |
|
AIMS OF REHABILITATION |
||
|
|
|
|
|
Decrease initial pain and inflammation. |
Identify biomechanical dysfunction. |
Improve flexibility. |
|
|
|
|
|
Strengthen the plantar fascia. |
Return to full fitness. |
Injury prevention. |
|
REDUCING PAIN AND INFLAMMATION |
||
|
||
|
RETURN TO PLAY |
||
|
||
| HOW CAN WE HELP | |
|
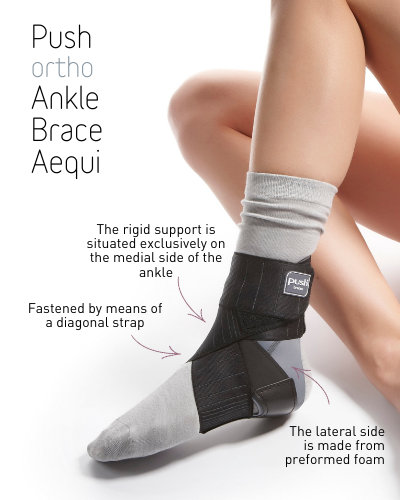
At Gateway Sports and Rehab we offer a wide range of ankle braces to aid in the recovery of ankle injuries, including our Push ortho Ankle Brace Aequi, an effective ankle orthosis which strikes the balance between efficient mechanical support of a disabled ankle and good wearer comfort. |
|
|
The rigid support is situated exclusively on the medial side of the ankle and has a recess for the malleolus. The lateral side is made from preformed foam, which easily adapts to the individual anatomy. The brace is fastened by means of a diagonal strap. Elastic straps apply pressure around the ankle. Inversion/eversion movement of the ankle is restricted while plantar/dorsal flexion is allowed adequate freedom. This means that no inhibition is felt during normal walking and running. The Push Aequi is worn over the sock, and optimal stabilisation can only be achieved if it is worn with a closed (laced-up) shoe. |
|
|
Read more on the Fraunhofer study and Push Aequi braces here - https://www.push.eu/aequi-study-jd-healthcare The study is to investigate the feasibility of a new dynamic testing method for ankle braces, to quantify the mechanical stability of different orthotic designs. A mechanical artificial foot model has been designed, considering the anatomy and biomechanics of the human foot. Sensors were built into the ankle joint, based on medical and technical principles. Together with an actuator, they were used as a test bench for validating ankle braces. For a first feasibility study, the influence of five different types of ankle orthoses for selected movement sequences was investigated. |
|
|
|
Need to be fitted before buying a Push Brace? Visit http://pushbraces.com.au/store-locator/ to find you nearest stockist. |
|
|
Need to be fitted before buying a Push Sports Brace? Visit http://www.pushsports.com.au/store-locator/ to find you nearest stockist. |
|
Please contact us if you would like more information on our product range on 1300 982 259 or fill in the contact form. |
|
| Ref: Sports Medicine Australia, Push Braces | |